So I reviewed the baby’s weight history (normal) and recent weight gain (great). The baby wasn’t getting nutrition, not even fluid, from any other source. So that must mean that Amy’s breasts are doing a great and normal job at keeping him healthy and thriving. There’s no evidence of any kind that her body will either suddenly or gradually stop providing the milk it has already proven that it can provide. She understood the logic, but didn’t have a lot of confidence for the future. She asked what would happen if, despite her excellent track record, she just failed to make enough or any.
What indeed, I asked her back. I guided her through this unlikely scenario the way we should plan a fire exit in our homes. First, would she know? She didn’t have confidence that she would, so I asked her how she would find out. She correctly figured that the baby would be hungry. Since her baby was neurologically normal, and since hunger is one of our most primitive and basic drives, the baby would surely let her know if he weren’t getting enough.
She wasn’t debating with me, but my answers gave her the freedom to ask the frightening questions without being judged harshly. What if the baby was crying and she couldn’t tell if it was from hunger and it really was but she didn’t know? OK, how long would you let the baby cry before calling me? She didn’t know exactly, but it was a lot less than a day. She agreed that her healthy baby could go a few hours without eating and still do well. If the baby really were crying inconsolably, I would always want to be called and usually want to see the baby in person. This is all pretty standard stuff, I think. As we went back and forth on this precise topic, however, I happened upon the answer she needed. I hadn’t understood exactly what would break through this until I hit upon it after trying other answers. 3 hours. That was the key, as it turned out. She was glad to get the reassurance, glad to get my commitment to be there if needed, confident in my professional skills and judgment. What she didn’t have was the confidence to trust her own common sense and innate ability to see when the baby has crossed over from fussy to worrisome. She needed an unambiguous border she could look for. If the baby crosses it, she knows exactly what to do. I could see the relief on her face when I said 3 hours. Any time, day or night, for any reason. Hunger, illness, bad weather, it just didn’t matter. If you try everything you know and the baby is crying for 3 hours, call me.
That wasn’t the only breakthrough. Like many new mothers I see, she was anxious about her continued ability to nurse successfully, even though she had been doing it perfectly. There are sometimes reasons that women have to stop, but they aren’t common. Usually, with some support and expert advice, breastfeeding problems can be overcome. But how, she wondered, does she really know that? She has already taken her body places it has never gone. Sure, my experience is optimistic, but that’s based on other women, other babies. This, I admitted, was an excellent point. I don’t push formula, but this is its perfect role. How do we know if 911 will answer when we call? Still, we teach even kids this number. That can of formula can usually sit on the shelf of a kitchen cabinet for a year. It can wait like a silent guardian, hidden behind the stuff you actually use. Nobody but you and your doctor need to know it was ever there. A can might feed a baby for several days or a week, depending on how big they are. But even if never touched until you throw it away when discovering it as you pack up to move, it is working its magic as an effective contingency plan. Depending on the disfavor in which formula is held, it might not be plan B or even C. But the one day when you decide to leave the baby with your mom for a few hours, but a truck got stuck under an overpass and there’s no way to get off the freeway and people are stopped and getting out of their cars, that can will be there.
Next, and I’ve made this point about bicycle helmets, protecting the baby might be a necessity but the safe and thriving baby is nowhere good without you. So taking care of yourself is crucial for the baby’s life and happiness.
 No, that doesn’t mean I think you should give in to the urge, ever since you heard of that big storm in the Gulf of Alaska, to have a neoprene Snugli custom made so that you'll be prepared when you get the text that Mavericks is up—way up—and you want to show the world how gnarly you really can be. Once the baby’s needs are met, we need to find a way to fold them into our lives in some functional way, or perhaps fold our lives into theirs. For Amy, this meant getting out of bed, out of the sweatpants and into regular attire and footwear. Another subtle advantage of housecalls, I made this suggestion to help her, not hurt her feelings. Perhaps doctors don't usually make fashion tips, but this was an essential precursor to the final note of this post.
No, that doesn’t mean I think you should give in to the urge, ever since you heard of that big storm in the Gulf of Alaska, to have a neoprene Snugli custom made so that you'll be prepared when you get the text that Mavericks is up—way up—and you want to show the world how gnarly you really can be. Once the baby’s needs are met, we need to find a way to fold them into our lives in some functional way, or perhaps fold our lives into theirs. For Amy, this meant getting out of bed, out of the sweatpants and into regular attire and footwear. Another subtle advantage of housecalls, I made this suggestion to help her, not hurt her feelings. Perhaps doctors don't usually make fashion tips, but this was an essential precursor to the final note of this post.This last is important because it facilitates the next important suggestion I made. She needed to take a walk. I strongly urged her to go for a walk with the baby in a stroller every day, without exception. Every part of this idea has a reason behind it. The feedback I've received has been so consistently good about it that it seems inexplicable for it never being mentioned in my training or textbooks.
The walk allows the new mother to get some exercise. Since this is often after spending at least a few days in bed, even previously fit mothers should take it easy at first. And for goodness sake, check with your OB who may have information about your stitches that I just don't. Studies have clearly shown that even a couple of days in bed decrease our fitness level. Together with some blood loss, you need to get back on your feet. Studies have also consistently shown that exercise improves our mood. People who get some exercise every day tend to sleep better, and some important functions of their body seem to work better. These include breathing and digestion.
The walk allows the mother to get some daylight. Amy hadn't left her bedroom much since leaving the hospital. Her planning for the baby had been so good, in fact, that her room had a changing table and baby supplies, a crib, swing, and so on. I noted this as her mood gradually lifted, and inquired when she planned to start using empty tissue boxes as slippers as Howard Hughes apparently did when he sealed himself in the penthouse of a casino he owned. Just because she was suffering didn't mean I couldn't make fun of her. Daylight, too, has been demonstrated to lift the mood and help regulate sleep.
Daylight is also helpful for the baby. It is directly therapeutic for jaundice, which baby Henry didn't have. But the baby had been living in a dark cave for 9 months. It needs daylight exposure (not direct sun, just daylight) to establish a day/night pattern. It also needs daylight to help provide vitamin D, which is activated by sunlight.
I specified using a stroller for several reasons. The jostling of the stroller is a natural pacifier, which many babies find soothing. Slings of many kinds can be great when doing many activities, especially in places with a lot of other people around, such as supermarkets. But the stroller takes the weight off. There's no extra weight on your back, no extra weight on your hips and knees and ankles. That will make the walk just a little easier, and make you able to walk a little bit longer than you might be able to with a sling or backpack carrier. It also gives you the luxury of stopping. If the baby's asleep, you could stop at a park bench. The stroller also moves the baby away from your body. This seems counterintuitive, since I certainly want you to hold and love your baby pretty much constantly. But it brings up the timing issue.
Take the daily walk at the baby's fussiest time. If your baby is consistently fussy in the late afternoon, say between 4:00 and 7:00PM, that's the time to go out. There aren't too many things more frustrating than trying and failing to comfort a fussy baby. It makes us feel helpless and doubt our ability to parent. But if the baby's basic needs are being met, and we know he'll be fussy in the late afternoon, that's the time he'll benefit from the calming effect of that walk in the stroller. If it's his fussiest time, he won't be right in your face, reminding you of your shortcomings as a parent. That, after all, is what adolescence is for.
 Like every new mother, or maybe at least the good ones, Amy said she was worried if her baby was getting enough. Henry was a week old, and I walked her through my iterative procedure to determine if he was getting what he needed. He was gaining weight appropriately. He was having lots of wet diapers. He was satisfied after nursing, and could be heard swallowing voraciously at every feeding. This was apparently an adequate response until she asked me if I thought he’d be alive in 6 months.
Like every new mother, or maybe at least the good ones, Amy said she was worried if her baby was getting enough. Henry was a week old, and I walked her through my iterative procedure to determine if he was getting what he needed. He was gaining weight appropriately. He was having lots of wet diapers. He was satisfied after nursing, and could be heard swallowing voraciously at every feeding. This was apparently an adequate response until she asked me if I thought he’d be alive in 6 months.
 When Amy called, she sounded fine. She’s in her early 30’s and just had her first child, a great and healthy baby named Henry. The baby was about a week old.
When Amy called, she sounded fine. She’s in her early 30’s and just had her first child, a great and healthy baby named Henry. The baby was about a week old.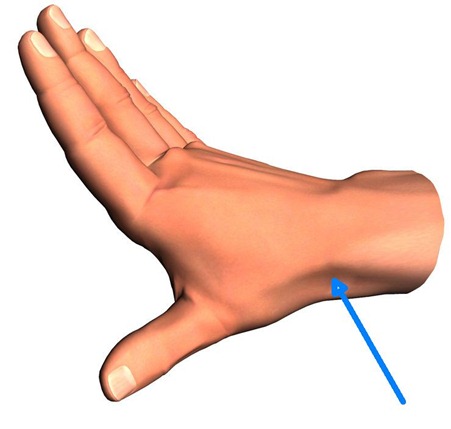


 perhaps, places where nursing is the exclusive source of child nutrition extending well beyond a year are usually places of great deprivation.
perhaps, places where nursing is the exclusive source of child nutrition extending well beyond a year are usually places of great deprivation.


 I gave the mother a pair of questionnaires I give to parents to help me evaluate anxiety disorders in children. The responses were convincing.
I gave the mother a pair of questionnaires I give to parents to help me evaluate anxiety disorders in children. The responses were convincing.





